TROPION-LUNG08
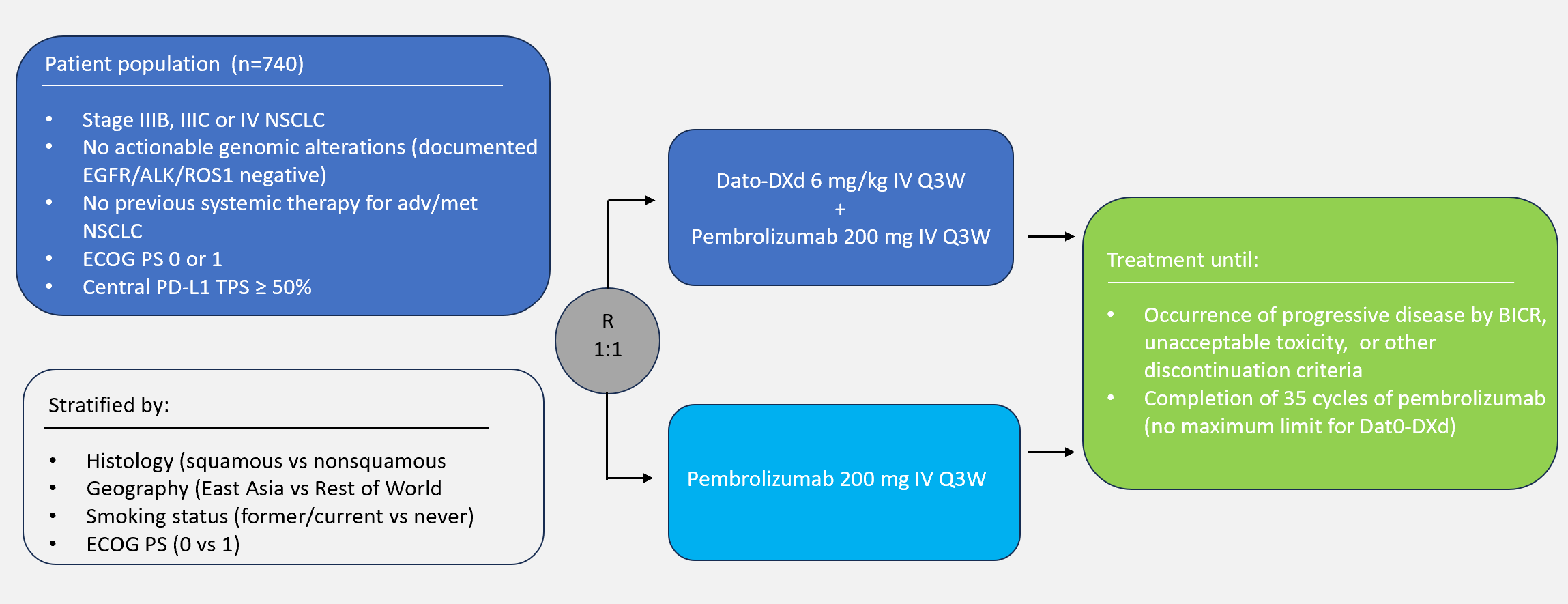
A Randomized, Open-label, Phase 3 Trial of Dato-DXd Plus Pembrolizumab vs Pembrolizumab Alone in Treatment-naïve Subjects with Advanced or Metastatic PD-L1 High (TPS ≥50%) NSCLC Without Actionable Genomic Alterations (Tropion-Lung08) (Dato-DXd Plus Pembrolizumab vs Pembrolizumab Alone in the First-line Treatment of Subjects with Advanced or Metastatic NSCLC Without Actionable Genomic Alterations)
Enrollment
Recruiting, extended until June 2024
No. of patients
0 / 740
Population
Subjects (≥18) with NSCLC without actionable genomic alterations, and with high PD-L1 expression (TPS ≥50%), and who have not previously received systemic therapy for advanced or metastatic NSCLC, or who have received neoadjuvant/adjuvant systemic therapy without ICIs and completed treatment at least 6 months prior to the diagnosis of advanced/metastatic disease
Design
A global, multicenter, randomized, open-label, active-controlled Phase 3 study
Approximately 740 eligible subjects will be randomized in a 1:1 ratio as indicated below:
- Arm 1: 200 mg pembrolizumab, followed by Dato-DXd (6.0 mg/kg), each administered on Day 1 of every 21-day cycle
- Arm 2: 200 mg pembrolizumab, administered on Day 1 of every 21-day cycle
Randomization will be stratified by Eastern Cooperative Oncology Group performance status (ECOG PS) (0 vs 1), histology (squamous vs non-squamous), geographical region (East Asia vs rest of world [ROW]) and smoking status former/current vs never).
No crossover between the 2 study treatment arms is permitted
Key outcome parameters
PFS and OS
Intervention
200 mg pembrolizumab & Dato-DXd or pembrolizumab alone
Key inclusion criteria
Inclusion criteria:
- Had an allogenic tissue/solid organ transplant
- Stage IIIB or IIIC disease and not candidates for surgical resection or definitive chemo radiation, or Stage IV NSCLC disease at the time of randomization
- Documented negative test results for EGFR, ALK, and ROS1 actionable genomic alterations based on analysis of tumor tissue. If test results for EGFR, ALK, and ROS1 are not available, subjects are required to undergo testing performed locally for these genomic alterations.
- No known actionable genomic alterations in NTRK, BRAF, RET, MET, or other actionable driver kinases with locally approved therapies. (Testing for genomic alterations besides EGFR, ALK, and ROS1 is not required prior to enrollment). Subjects with squamous NSCLC are only required to undergo EGFR, ALK, and ROS1 testing if they have no history of tobacco smoking or were diagnosed with NSCLC at <40 years of age.
- Subjects whose tumors harbor KRAS mutations are eligible for the study.
- Tumor has high PD-L1 expression (TPS ≥50%) as determined by PD-L1 IHC 22C3 pharmDx assay by central testing (minimum of 6 slides).
- Has provided a formalin-fixed tumor tissue sample (minimum of 10 [preferably 15] × 4-micron sections or block equivalent) for the measurement of TROP2 protein expression and for the assessment of other exploratory biomarkers. This tissue requirement is in addition to the tissue required for PD-L1 testing for tissue screening purposes.
- Has left ventricular ejection fraction (LVEF) ≥50% by either an echocardiogram (ECHO)or multigated acquisition scan (MUGA) within 28 days before randomization.
- ECOG PS of 0 or 1 at screening
Key exclusion criteria
Exclusion criteria:
- Has received prior systemic treatment for advanced/metastatic NSCLC
- Has received prior treatment with any of the following, including in the adjuvant/neoadjuvant setting:
- Any agent, including an ADC, containing a chemotherapeutic agent targeting topoisomerase I
- TROP2-targeted therapy
- Any anti-PD-1, anti-PD-L1, or anti-PD-L2 agent or with an agent directed to another stimulatory or co-inhibitory T-cell receptor (eg, CTLA-4, OX40, CD137)
- Any other ICIs
- Subjects who received adjuvant or neoadjuvant therapy OTHER than those listed above, are eligible if the adjuvant/neoadjuvant therapy was completed at least 6 months prior to the diagnosis of advanced or metastatic disease
- A computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the brain at baseline (MRI preferred) is required for all subjects
- Has received prior radiotherapy ≤4 weeks of start of study intervention or more than 30Gy to the lung within 6 months of Cycle 1 Day 1
- History of another primary malignancy (beyond NSCLC) except for:
- Malignancy treated with curative intent and with no known active disease ≥3 years before the first dose of study treatment and of low potential risk for recurrence
- Adequately treated non-melanoma skin cancer or lentigo maligna without evidence of disease
- Adequately treated carcinoma in situ without evidence of disease
- Participants with a history of prostate cancer (tumor/node/metastasis stage) of Stage ≤T2cN0M0 without biochemical recurrence or progression and who in the opinion of the Investigator are not deemed to require active intervention
- Malignancy treated with curative intent and with no known active disease ≥3 years before the first dose of study treatment and of low potential risk for recurrence.
- Adequately treated non-melanoma skin cancer or lentigo maligna without evidence of disease.
- Adequately treated carcinoma in situ without evidence of disease.
- Participants with a history of prostate cancer (tumor/node/metastasis stage) of Stage ≤T2cN0M0 without biochemical recurrence or progression and who in the opinion of the Investigator are not deemed to require active intervention.
- Uncontrolled hypertension (resting systolic blood pressure >180 mmHg or diastolic blood pressure >110 mmHg) within 28 days before randomization.
- Significant corneal disease.
- Had an allogeneic tissue/solid organ transplant
Contact opnemen over een studie
Neem contact op voor meer informatie over de studies van de afdeling thoracale oncologie van Amsterdam UMC.